
This chapter will emphasise the need to: 1) Provide a provisional restoration following tooth preparation to protect the pulp; secure positional stability, function and aesthetics; and maintain gingival health; 2) Consider using long-term provisional restorations to assess aesthetic, occlusal and periodontal changes before embarking on definitive restorations; 3) Distinguish between preparations for conventional and adhesive restorations when providing provisional restorations; 4) Determine in advance the type of provisional restorations and materials to be used, ideally, while treatment planning; 5) Be aware of materials for making provisional restorations and how to control potential hazards; and 6) Make provisional restorations to a high standard to ensure a predictable restorative outcome.



After completing tooth preparation (Chap. 20), you will routinely want to provide your patient with a provisional restoration.
The terminology surrounding this stage of treatment can be confusing. The Glossary of Prosthodontic Terms 1 considers the terms 'provisional, temporary and interim' to be used interchangeably and describes a prosthesis that is 'designed to enhance aesthetics, stabilisation and/or function for a limited period of time, after which it is to be replaced by a definitive prosthesis'. For the purposes of consistency, we will use the terms 'provisional restoration' or 'provisional'.
Not only can good provisional restorations help to produce better final restorations, they can also save a lot of time and expense at subsequent appointments. This chapter discusses the need for provisional restorations, the various types and the many materials available for construction. Provisional restorations for adhesive definitive restorations often pose a difficult problem, and these are considered towards the end of the chapter, along with other commonly encountered problems.
The various functions fulfilled by provisional restorations are described in Table 1. When constructing provisional restorations for a full crown preparation, the two essentials are to cover freshly cut dentine (strangely not emphasised in the above definition) and prevent tooth movement. With minimal preparations for adhesive restorations, protection of prepared enamel is usually less of an issue, and often a provisional restoration is not needed unless it is important to prevent unwanted tooth movement or maintain aesthetics.

It is sometimes forgotten that provisional restorations can help stabilise periodontal condition before definitive restoration. They also have diagnostic uses; for example, testing aesthetic and occlusal changes before they are incorporated in a definitive restoration. These important uses are considered next.
It may be necessary as part of a patient's periodontal management to remove overhanging restorations to allow access for cleaning and resolution of inflammation (see Chaps. 4 and 10). Long-term wear of properly fitting and contoured provisional restorations allows the health of the gingival margin to improve and its position to stabilise before impressions are recorded for definitive restorations, bearing in mind that this will occur faster in some patients than others (Fig. 2).

Following periodontal or apical surgery, the tissues will also need time to stabilise before the final finish line is cut for definitive crowns. Where surgical crown lengthening is used to increase clinical crown height, try to leave six months before definitive restoration, particularly if the aesthetics are critical (see Chap. 10). Provisional restorations can be provided soon after crown lengthening, but make sure they are durable and avoid finishing the preparations subgingivally as this may set up a chronic gingivitis which is difficult to resolve.
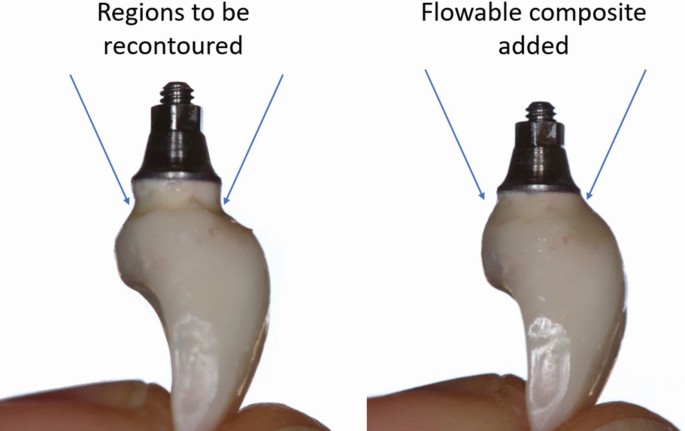
With implant abutments (see Chap. 16), the surrounding gingival tissues may be 'sculpted' four months after implant placement to improve aesthetics by enhancing the emergence profile and interproximal papillae. 2 This is done with screw-retained provisional restorations which are contoured chairside by adding flowable composite 3 or acrylic resin 4 to the subgingival portion of the provisional restoration (Fig. 3). This exerts 'dynamic pressure', in other words a sustained but diminishing pressure, against the inner aspect of the tissue. While undoubtedly a useful technique, there are limits to what can be achieved which are covered in Chap. 17.
Provisional restorations, especially those used for crown preparations, are invaluable where aesthetic, occlusal or periodontal changes are planned. The principles behind such changes are discussed below.
Proposed changes to the shape of the anterior teeth are best tried out with provisional restorations to ensure patient acceptance and approval from friends and family. It's much easier to trim or add acrylic than ceramic. Once happy, an alginate is recorded so that the technician can copy the desired shape into the definitive restoration. If only one or two teeth are involved, some dentists prefer to contour provisional restorations at the chairside, but with multiple restorations, clinical time can be saved by having a diagnostic wax-up and matrix made in the laboratory (Fig. 4). Alternatively, indirect provisional restorations can be prescribed which will be described later.
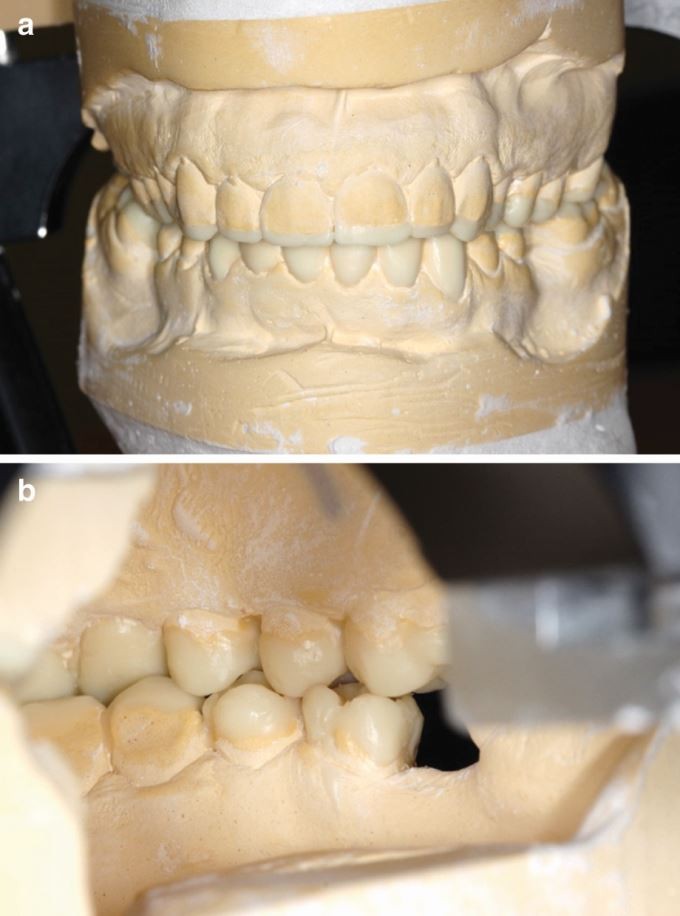
If you want your extra-coronal restorations to change a patient's anterior guidance or increase the occlusal vertical dimension, it's worth trying out the changes first with provisional restorations. The occlusal changes are best planned (see Chap. 12) with a diagnostic wax-up using casts mounted on a semi-adjustable articulator (Fig. 5). From the wax-up a matrix can be made to mould diagnostic provisional restorations either directly or indirectly. After fitting and adjusting, they are temporarily cemented. The adjustment should provide even occlusal contact in the intercuspal position and guidance or disclusion as required. The patient can then be examined at a further appointment and the occlusal surfaces copied if the following criteria are met:

There are several ways of copying guidance surfaces between provisional and definitive restorations. We prefer to use a custom guidance table as described in Chap. 12.
Where a patient's occlusal vertical dimension needs to be increased, it is often wise to make an initial assessment (for example, with a stabilisation splint) before the teeth are irreversibly prepared. However, this stage is less important if the teeth are to be restored with direct composite restorations. This is because composite can easily be adjusted and added to intraorally.
For most people, minor adjustments in tooth shape are unlikely to cause any problems, but for others, for example, singers and wind instrument musicians, the eventual restorations, if poorly planned, may interfere with a patient's 'embouchure'. This term describes the fine mouth movements and lip/tooth contact required for speech pro-duction or sound generation in the case of a musical instrument. Also, the incorporation of wider cervical embrasure spaces, to facilitate interproximal cleaning, may occasionally cause embarrassment due to air leakage. Therefore, it makes sense to copy the features of successful provisional restorations to avoid patient dissatisfaction and expensive remakes.
As a guide to the maze of different provisional restorations, we first need to consider the materials and then the techniques by which they are formed. Most provisionals are formed directly in the mouth, but for long-term wear or diagnostic use, indirect provisional restorations have advantages and can be fashioned either in the lab or, where facilities exist, in the surgery. Impressions can either be conventional or optical (Chap. 22).
It is worth emphasising that the time between preparation of the teeth and cementation of final restorations can vary from a few days for straightforward cases (short-term) to several weeks (medium-term) or even, in the case of complex reconstruction, several months (long-term). The longer provisional restorations are in the mouth, the greater are the demands on the material from which they are made.
There are materials for direct use intra-orally and materials for making provisional restorations indirectly, either in the lab or in suitably equipped dental surgeries. Materials for direct use comprise preformed crowns (made of plastic or metal) and an increasingly wide range of specially formulated resins and resin composites (see Table 2). In the lab, provisional restorations are generally made in self-cured or heat-cured acrylic, composites or cast metal. CAD/CAM may also be used to mill provisional restorations from polymerised resin blanks (see Chap. 14).

Look again at Table 2 and we will consider materials from a historical perspective.
In the 1960s, provisional crowns were made from self-cured polymethyl methacrylate (PMM) - a material which continues to be used by some dentists. PMM is strong, has relatively good wear resistance, can be easily added to, and has good aesthetics which lasts well for long-term use. However, it does have significant disadvantages:
It is, however, a good material for indirect provisional restorations made either chairside or in the laboratory. To reduce porosity, self-cured acrylic can be polymerised under pressure in a hydroflask. 8 Alternatively, the lab can use heat-cured acrylic.
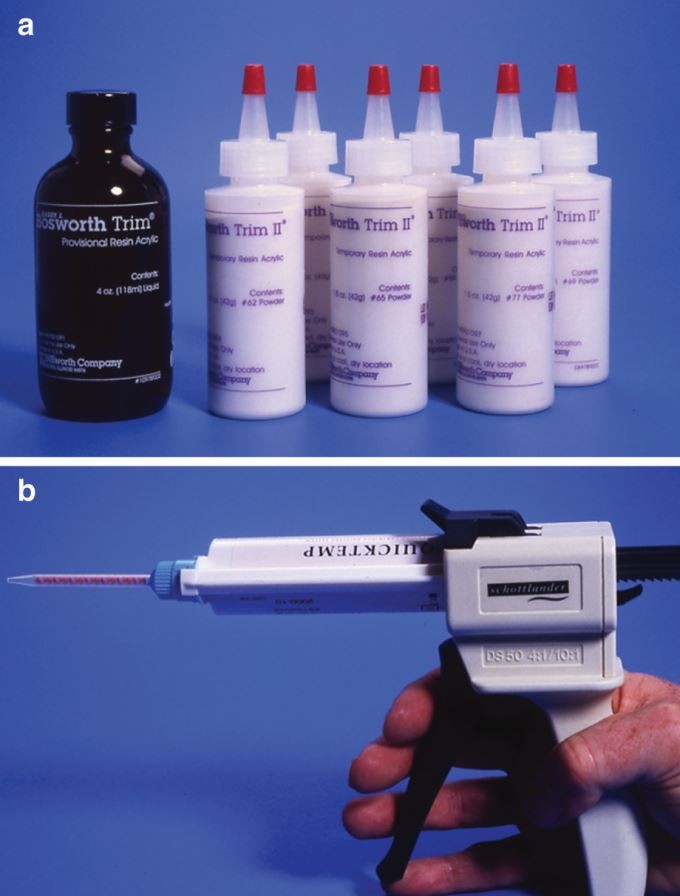
Polyethyl methacrylate (PEM) (see Figure 7a) was introduced in the 1970s specifically for intraoral use because it shrinks less and is less exothermic than PMM. However, strength, wear resistance, aesthetics and colour stability are not as good. Most presentations come with a wide colour range (eg Trim II, Keystone Industries, has six shades). These materials contain a phthalate plasticiser which may leach out of the set material. 6 , 9 Phthalates are considered as endocrine disruptor chemicals that can cause oestrogenic behaviour and are possible carcinogens. 10 The level of risk posed to patients by eluents from temporary restorations is unclear.
Over the past two decades, manufacturers have introduced several developments in the formulation and presentation of composite materials used for provisional restorations.
Bis-acryl composites gained popularity in the 1980s largely due to the convenient mixing system: automix syringes (see Figure 7b), which provide a consistent and air-free product. Unfortunately, it is difficult to define exactly what is meant by bis-acryl. A broad-brush definition says it comprises: 'Monomers such as bisphenol-A-glycidyl methacrylate (bis-GMA), triethylene glycol dimethacrylate (TEGDMA) or similar monomer systems derived from Bowen resin'. 11 Clearly, there is endless scope for manufacturers to adjust constituents and their concentrations - so one bis-acryl material may have very different properties to another. Indeed, the early materials (for example, Protemp, ESPE-Premier) produced less heat and shrinkage during polymerisation than other resins, making them more pulp-friendly and resulting in a better marginal fit. 7 However, despite being reasonably strong, they were brittle in thin sections and difficult to add to. They also stained easily if the unpolymerised surface layer was not removed with an alcohol wipe and polishing.
To illustrate how some bis-acryl materials have changed over the past ten years, Quicktemp (Schottlander) provides a good example evolving first into Quicktemp II and then Quicktemp Cosmetic. The manufacturer claims Quicktemp II has a revised formulation giving improvements in strength, hardness and aesthetics 12 but seemingly at the expense of an exotherm approaching 50 °C. 6 Quicktemp Cosmetic is claimed to have further significant improvements in mechanical properties by including a large component of urethane diacrylate (UDMA). While tempting to use the stronger 'cosmetic' material for all purposes, it has an even higher exotherm than Quicktemp II. 13 So, to avoid overheating a vulnerable pulp, it is important to remove the partly set material from the mouth before reaching the exothermic reaction.
As a rule, bis-acryl resins appear more colour stable than PEM materials and better suited for use as long-term provisionals. 7 However, they will not form a reliable chemical bond to themselves or to flowable composite resins which may be needed for repairs and additions after intraoral curing. Nevertheless, priming the defect with a resin bonding agent provides a reliable solution to this problem. 14 Indeed, Quicktemp Cosmetic provides an unfilled resin and a light-cured UDMA composite in a range of four shades. The resin bonding agent can also be used as a surface glaze. 13
Bis-acryl composite (dual-cured) - the development of stronger bis-acryl resins has not only involved reformulations of resin and filler content but also methods of setting. TempSpan, SYNCA, is a syringe-mixed material which can also be light-cured. Such dual curing is popular as it saves clinical time, but take care not to lock in restorations and cause a seared pulp: light-curing generally creates a higher exotherm than self-curing because of the greater speed of reaction and the additional heat from the curing light. 15
Malleable composites - these are light-cured composites with a clay- or dough-like consistency allowing them to be moulded over a tooth prep and then cured. The simplest system, Revotek LC, GC, consists of a UDMA putty stick from which a portion can be cut. A more sophisticated approach is for the composite dough to be supplied preformed as a crown (eg Protemp, 3M ESPE Crown Temporization Material, made, in part, from Bis-GMA). 11
Restorative composites - these are normally used for definitive restorations but can be used as a provisional material for adhesive preparations (eg for veneer preps), as described later. Dentists sometimes heat composites to reduce viscosity and make them easier to mould 16 or use with a matrix. There are also light-cured and dual-cured composites designed for laboratory fabrication which may also be useful for long-term provisional restorations.
All the above resin-based materials have an exothermic reaction and if used directly may have implications for the pulp, particularly if the material is not removed from the mouth at the appropriate time. Currently, there is no ISO standard specifying an upper limit to the exotherm from these materials, which some may find surprising.
Dentists enthusiastic about CAD/CAM technology (see Chap. 14) will be delighted to know that highly accurate provisional restorations can be milled from blanks made from a variety of prepolymerised resins including PMM, polyetheretherketone (PEEK) and acetate. 17 Some materials may perform better than others; under conditions of simulated crown loading, the fracture strength of PMM and PEEK was significantly higher than for acetate and the comparator - a syringe-mixed bis-acryl composite.
Cast metals are hardly ever used for provisional restorations but are mentioned for completeness. They are very durable and may occasionally be used for long-term provisionals in bruxists.
The BDJ Editorial Team would like to thank the authors of this chapter for granting us permission to republish their chapter within our journal. This chapter was first originally published in R. Wassell et al. (eds), Extra-Coronal Restorations, BDJ Clinician's Guides, https://doi.org/10.1007/978-3-319-79093-0_23 © Springer International Publishing AG, part of Springer Nature 2019. The second half of this chapter will be republished in an upcoming issue of the BDJ.